Summary
Pelvic floor dysfunction (PFD) affects millions of Canadians, causing symptoms ranging from urinary problems to chronic pain and intimacy issues. This condition stems from various causes including injuries, aging, childbirth, and neurological disorders. Understanding the symptoms helps distinguish PFD from similar conditions like interstitial cystitis or IBS, enabling proper diagnosis and effective treatment strategies.
Are you experiencing unexplained pelvic discomfort, persistent bathroom urgency, or intimacy problems that disrupt your daily life? These symptoms often signal pelvic floor dysfunction, a treatable condition affecting the muscles supporting your pelvic organs.
Many people suffer silently for years, believing these symptoms are just something to endure or feeling too embarrassed to seek help. The good news is that most pelvic floor issues respond well to proper treatment approaches. Tools like a pelvic toner device can play a key role in strengthening weakened muscles. Learning to recognize the signs and understand their causes is your first step toward finding relief and reclaiming comfort in your daily activities.
What Are the Key Symptoms of Pelvic Floor Dysfunction
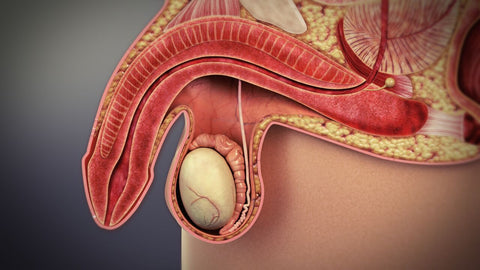
Pelvic floor dysfunction causes difficulty in controlling muscles that support the bladder, bowel, or uterus. Key symptoms include urinary incontinence, pelvic pain, painful intercourse, and constipation. Causes range from childbirth, surgery, chronic constipation, and aging to nerve damage or trauma.
Frequent Bathroom Visits
PFD often creates an intense urge to urinate throughout the day. This urgency can disrupt daily activities and leave you feeling anxious about bathroom access.
Many individuals also experience nocturia, waking multiple times at night to empty their bladder. Additionally, you might feel like your bladder hasn't completely emptied despite just using the bathroom.
These symptoms occur because the pelvic floor muscles cannot properly relax during urination. As a result, normal bladder function becomes compromised, creating a frustrating cycle of bathroom visits.
Bowel Problems
PFD commonly causes constipation and difficult bowel movements. You might find yourself straining excessively or feeling like elimination is incomplete afterward.
Many people need to change positions or use manual assistance to complete bowel movements. This happens because tight or uncoordinated pelvic floor muscles prevent proper relaxation during elimination.
The problem often creates a challenging cycle of worsening symptoms. Consequently, chronic constipation increases muscle tension, which further exacerbates the pelvic floor dysfunction.
Pelvic Pain
Chronic pelvic pain frequently signals PFD, appearing as discomfort in the lower abdomen, genitals, or rectum. The pain may be constant or occur during specific activities like sitting, exercise, or intercourse.
This discomfort typically stems from muscle spasms and tension within the pelvic floor. Over time, sensitive trigger points develop in the muscles, creating referred pain patterns throughout the pelvis.
Effective treatment requires addressing both the physical muscle dysfunction and pain signals. Therefore, a combination of physical therapy and pain management techniques often provides the best relief.
Sexual Dysfunction
PFD can significantly impact intimate relationships by causing pain during intercourse. Women may experience discomfort or burning sensations, while men might develop erectile difficulties or pain with ejaculation.
The underlying cause involves inability of pelvic floor muscles to properly contract and relax during sexual activity. Furthermore, anticipation of pain often creates anxiety, which tensens muscles further and worsens symptoms.
Sexual dysfunction from PFD affects not just physical intimacy but emotional wellbeing too. Fortunately, specialized pelvic floor therapy can substantially improve function and comfort during intimate moments.
Leaking Urine
Urinary incontinence—leaking urine unexpectedly—is perhaps the most common symptom of PFD. This typically happens during coughing, laughing, sneezing, or physical activities that increase abdominal pressure.
The leakage occurs because weakened pelvic floor muscles cannot properly support the bladder. As a result, even minor pressure changes overcome the compromised sphincter control.
Beyond physical discomfort, this symptom often causes embarrassment and social withdrawal. However, targeted exercises and proper training can significantly improve bladder control and restore confidence.
Causes of Pelvic Floor Dysfunction
Understanding the underlying causes of PFD is essential for prevention and effective treatment. Various factors, ranging from physical trauma to lifestyle habits, can contribute to the development of this condition. Identifying your specific risk factors helps create tailored treatment plans for better outcomes.
Traumatic Injuries to Your Pelvic Area
Physical trauma can directly damage the delicate structures of your pelvic floor. Car accidents, falls, or sports injuries may tear muscles or injure nerves that control pelvic function.
These injuries often disrupt the normal coordination between muscles and nerves. Consequently, even after the initial trauma heals, lasting dysfunction can persist without proper rehabilitation.
Prompt medical attention after pelvic injuries is crucial for recovery. Therefore, reporting any pelvic pain or dysfunction following an accident can prevent long-term complications and improve treatment success.
Overusing Your Pelvic Muscles
Certain habits can place excessive strain on your pelvic floor over time. Frequent heavy lifting, chronic constipation, or persistent coughing creates repetitive pressure that weakens these muscles.
Many people unknowingly hold tension in their pelvic floor during stress. This constant clenching, similar to jaw tension, eventually exhausts the muscles and leads to dysfunction.
Exercise choices can also contribute to overuse problems. High-impact activities without proper form or adequate rest periods may damage pelvic floor muscles, especially if core strength is insufficient.
Surgery
Pelvic surgeries can inadvertently affect the muscles and nerves controlling your pelvic floor. Procedures like hysterectomies, prostatectomies, or colorectal operations may disrupt the normal anatomy.
Surgical scarring can restrict movement and create tension in the pelvic region. Moreover, nerve damage during surgery might impair the signals that coordinate proper muscle function.
Post-surgical rehabilitation is often overlooked but critically important. Therefore, working with specialists who understand pelvic floor recovery can significantly improve outcomes after pelvic surgeries.
Aging
Natural aging processes affect all muscles in the body, including the pelvic floor. Muscle fibers gradually lose strength and elasticity as we age, making dysfunction more common.
Hormonal changes, particularly declining estrogen during menopause, further impact tissue quality. As a result, the supportive structures become thinner and less resilient to daily pressures.
Preventative care becomes increasingly important with age. Fortunately, regular pelvic floor exercises and appropriate lifestyle modifications can significantly slow age-related changes and maintain function.
Neurological Conditions
Certain neurological disorders directly impact the nerve signaling to pelvic floor muscles. Multiple sclerosis, Parkinson's disease, or stroke can disrupt the brain's ability to control these muscles properly.
Spinal cord injuries may sever critical nerve pathways to the pelvic region. Consequently, this interruption prevents normal muscle coordination during bladder and bowel function.
Diabetes and other conditions affecting peripheral nerves also contribute to dysfunction. Over time, nerve damage from these conditions reduces sensation and control, complicating both diagnosis and treatment of pelvic floor issues.
Pregnancy and Childbirth
The physical demands of pregnancy place significant strain on the pelvic floor muscles. As the baby grows, increasing weight and pressure stretch these muscles beyond their normal capacity.
Vaginal delivery can further traumatize the pelvic floor structures. During birth, muscles may tear or stretch excessively, and nerves might become compressed or damaged.
Multiple pregnancies or births involving forceps or large babies increase risk factors. However, proper prenatal preparation and postpartum rehabilitation can significantly reduce long-term pelvic floor problems.

Conditions That Can Be Mistaken for Pelvic Floor Dysfunction
Diagnosing pelvic floor dysfunction can be challenging because symptoms often overlap with other conditions. Many patients receive incorrect diagnoses and treatments before discovering pelvic floor issues are the root cause.
Proper diagnosis requires thorough evaluation by healthcare providers familiar with pelvic health. Unfortunately, many medical professionals have limited training in recognizing PFD specifically.
The path to correct diagnosis often involves ruling out other possibilities first. Therefore, understanding conditions with similar presentations can help advocate for appropriate testing and referrals.
Several medical conditions present symptoms that mimic pelvic floor dysfunction:
-
Interstitial Cystitis/Bladder Pain Syndrome – This chronic bladder condition causes pelvic pain and frequent urination similar to PFD but originates from bladder tissue inflammation rather than muscle dysfunction.
-
Endometriosis – Tissue similar to the uterine lining grows outside the uterus, causing pelvic pain that may be confused with PFD pain patterns, especially during menstruation or intercourse.
-
Irritable Bowel Syndrome (IBS) – The bowel symptoms of IBS, including constipation and abdominal discomfort, can closely resemble the digestive manifestations of pelvic floor problems.
-
Prostatitis – In men, inflammation of the prostate gland creates pelvic pain and urinary symptoms that mimic pelvic floor tension and dysfunction.
Take Control of Your Pelvic Health with Trusted Solutions
At Urology Health Store Canada, we understand the challenges that come with pelvic floor dysfunction. That’s why we offer a carefully curated range of clinically trusted products designed to support your recovery journey.
From advanced electronic pelvic toners like the Kegel8 Ultra 20 V2 to effective biofeedback devices such as the NeuroTrac® MyoPlus Pro, our solutions empower both men and women to strengthen pelvic floor muscles, manage incontinence, and reduce chronic pelvic pain—all from the comfort of home.
But we go beyond just products. We're committed to educating and supporting our customers with expert guidance and resources. Our website features informative blogs, trusted pelvic health clinics, and tools to help you make informed decisions about your health.
With discreet shipping, expert-recommended solutions, and a customer-first approach, Urology Health Store Canada is your dedicated partner in achieving better pelvic health.